Nurses’ Technology Acceptance of Electronic Health Record and Its Perceived Efficiency in Patient Care: A Basis for Evidence-Informed System Enhancement
DOI:
https://doi.org/10.65232/w4p71w68Keywords:
Electronic Health Record, Nursing Efficiency, Technology Acceptance, Patient Care, TrakCareAbstract
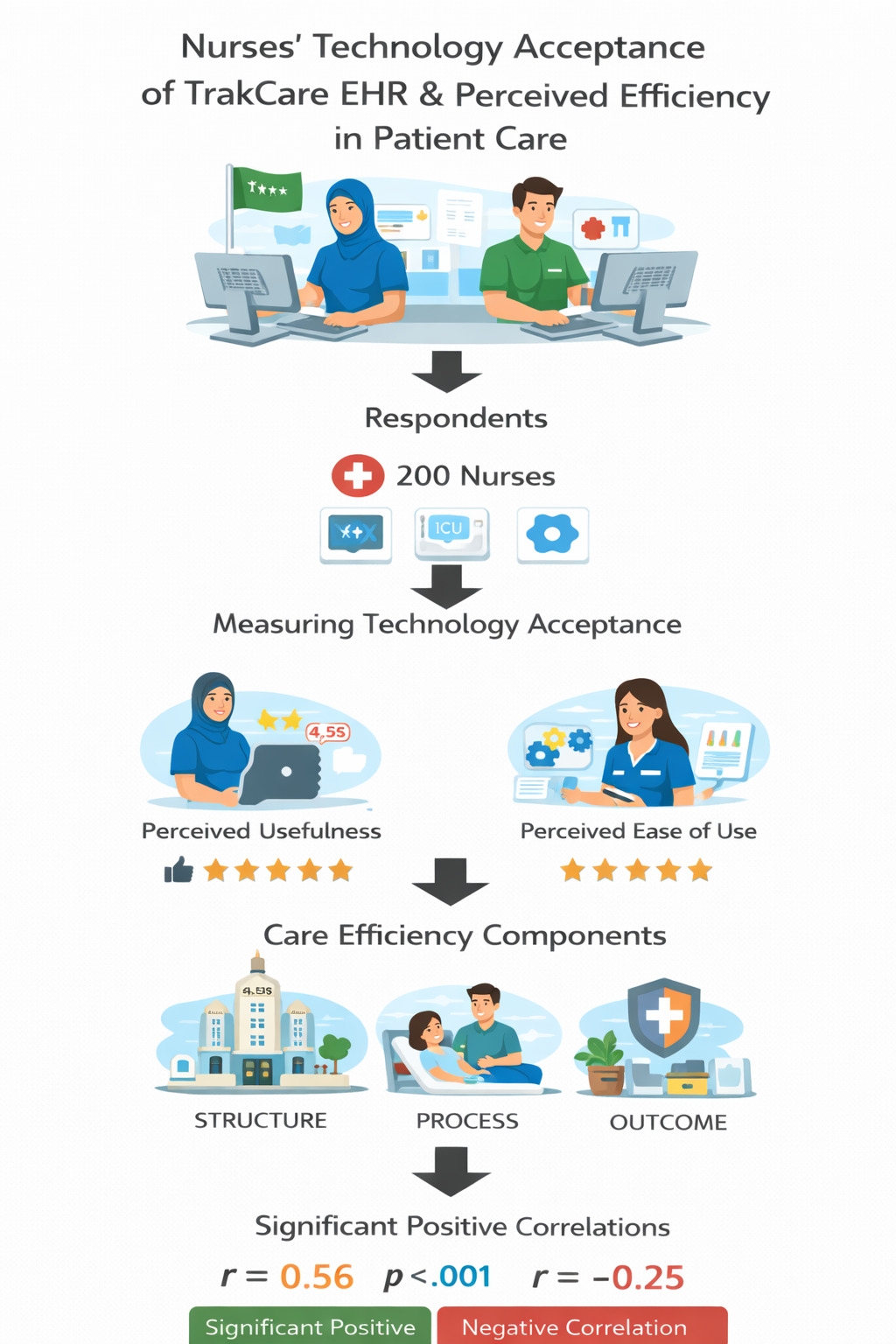
This study examined nurses’ technology acceptance of the TrakCare Electronic Health Record (EHR) system and its relationship with perceived efficiency in patient care in a tertiary hospital in Saudi Arabia. Using a descriptive correlational design, the study involved 200 nurses from emergency, intensive care, and general ward units. A validated four-part questionnaire measured perceived usefulness, perceived ease of use, and efficiency based on Donabedian’s structure–process–outcome model. Findings revealed that nurses strongly agreed that TrakCare enhances job performance and documentation accuracy. Perceived ease of use was rated agreeably, although several items—particularly error recovery—were rated lower, indicating usability challenges. Perceived usefulness and perceived ease of use were significantly correlated with structure and process components of care efficiency. A negative correlation was noted between perceived usefulness and tagging workload, suggesting that documentation burden may diminish perceived system value. These results underscore the need for continuous training, workflow-aligned system improvements, and usability enhancements to strengthen EHR-supported clinical performance. Evidence-informed system refinements are recommended to optimize nursing efficiency and promote better patient care outcomes.
Downloads
References
Aggarwal, A. (2025, August 25). InterSystems TrakCare implementation - Planit. Planit. https://www.planit.com/intersystems-trakcare-implementation/
Al-Kahtani, N. H., Khan, R. U., & Al-Kahtani, S. H. (2022). Electronic health records in Saudi Arabia: Challenges and recommendations. Healthcare, 10(2), 278. https://doi.org/10.3390/healthcare10020278
Al-Khalifa, H. S., & Al-Salman, A. S. (2020). Exploring the adoption and effectiveness of electronic health records in Saudi Arabia: A systematic review. International Journal of Medical Informatics, 141, 104241. https://doi.org/10.1016/j.ijmedinf.2020.104241
Al-Muammar, S. A., Al-Awaji, N., & Al-Harbi, S. (2020). User experience and satisfaction with electronic health records in Saudi Arabia: A cross-sectional study. BMC Medical Informatics and Decision Making, 20(1), 1–9. https://doi.org/10.1186/s12911-020-01184-3
Albagmi, F. M., Al-Moteri, M. A., & Thomas, D. (2022). Factors affecting nurses' intention to use electronic health records in Saudi Arabia: A structural equation modeling approach. BMC Medical Informatics and Decision Making, 22(1), 142. https://doi.org/10.1186/s12911-022-01931-y
Alharbi, M. M., Alqahtani, A. M., & Aljohani, F. S. (2022). Barriers to the adoption of electronic health records among nurses in Saudi Arabia. Journal of Multidisciplinary Healthcare, 15, 1067–1077. https://doi.org/10.2147/JMDH.S350831
Alhur, H. S. (2023). The impact of electronic health record usability on nurses’ job performance in Saudi Arabia. International Journal of Global Health and Research, 2(1), 88–100.
Almalki, A. M. O., & Alamri, F. B. H. (2025). The role of urgent care clinics in alleviating emergency department congestion: A systematic review of patient outcomes and resource utilization. Cureus, 17(4), e81919. https://doi.org/10.7759/cureus.81919
Alnaim, M., & Abou Hashish, E. A. (2021). Nurses’ perceptions of electronic health records implementation: Barriers and facilitators in Saudi Arabia. Informatics in Medicine Unlocked, 23, 100526. https://doi.org/10.1016/j.imu.2021.100526
Alobayli, F. (2023). Impact of electronic health records on nursing burnout in a hospital setting in Saudi Arabia: Mixed-methods study. JMIR Human Factors, 10, e49006. https://doi.org/10.2196/49006
Alqarni, A. A., Alharbi, R., & Alotaibi, R. M. (2021). Exploring nurses’ acceptance of health information technology in Saudi Arabia using the Technology Acceptance Model. Computers, Informatics, Nursing, 39(7), 389–397. https://doi.org/10.1097/CIN.0000000000000715
Alqurashi, M. M., Thobaity, A. A., Alzahrani, F., & Alasmari, H. A. (2022). Nurses’ experiences with an electronic tracking system in the emergency department: A qualitative study. Nursing Research and Reviews, 12, 223–234. https://doi.org/10.2147/nrr.s384136
Alrasheeday, A. M., Al-Rawashdeh, N., Alharbi, M. A., & Alotaibi, T. N. (2023). Nurses’ attitudes and factors affecting use of electronic health records in Saudi Arabia. Journal of Nursing Management, 31(2), 457–465. https://doi.org/10.1111/jonm.13776
Alsabaan, M., Almuayqil, A., & Alturki, R. (2020). A usability evaluation of EHR systems in Saudi Arabia: Challenges and recommendations. Journal of Infection and Public Health, 13(10), 1538–1542. https://doi.org/10.1016/j.jiph.2020.07.012
Alsulami, H., Conroy, S., & Choonara, I. (2019). Nurses’ perceptions of electronic health record implementation in Saudi hospitals: A qualitative study. BMC Nursing, 18(1), 1–9. https://doi.org/10.1186/s12912-019-0350-8
Austin, E., Blakely, B., Salmon, P., Braithwaite, J., & Clay-Williams, R. (2021). Identifying constraints on everyday clinical practice: Applying work domain analysis to emergency department care. Human Factors, 64(1), 74–98. https://doi.org/10.1177/0018720821995668
Bahlibi, T. T., Tesfamariam, E. H., Andemeskel, Y. M., & Weldegiorgis, G. G. (2022). Effect of triage training on the knowledge application and practice improvement among the practicing nurses of the emergency departments of the National Referral Hospitals, 2018; a pre-post study in Asmara, Eritrea. BMC Emergency Medicine, 22(1). https://doi.org/10.1186/s12873-022-00755-w
Bakhoum, N., Gerhart, C., Schremp, E., Jeffrey, A. D., Anders, S., France, D., & Ward, M. J. (2021). A time and motion analysis of nursing workload and electronic health record use in the emergency department. Journal of Emergency Nursing, 47(5), 733–741. https://doi.org/10.1016/j.jen.2021.03.007
Batko, K., & Ślęzak, A. (2022). The use of Big Data Analytics in healthcare. Journal of Big Data, 9(1), 3. https://doi.org/10.1186/s40537-021-00553-4
Cahill, J., Cleary, S., & Cullinan, J. (2025). Electronic health record usability and error recovery: Challenges for clinical staff. Journal of the American Medical Informatics Association, 32(1), 23–31. https://doi.org/10.1093/jamia/ocae213
Calder-Sprackman, S., Zhao, H., Devine, L. A., & Fitzpatrick, J. (2021). The impact of adoption of an electronic health record on emergency physician work: A time motion study. JACEP Open, 2(1), e12362. https://doi.org/10.1002/emp2.12362
Donabedian, A. (2005). Evaluating the quality of medical care. The Milbank Quarterly, 83(4), 691–729. https://doi.org/10.1111/j.1468-0009.2005.00397.x
Doolan-Noble, F., Lyndon, M., Hill, S., & Gray, J. (2020). Electronic health records and their impact on patient care: A review of the evidence. Health Information Management Journal, 49(1), 30–38. https://doi.org/10.1177/1833358319851689
El Mahalli, A. A. (2015). Adoption and barriers to adoption of electronic health records by nurses in three governmental hospitals in Eastern Province, Saudi Arabia. Perspectives in Health Information Management, 12(Winter), 1–18. https://pmc.ncbi.nlm.nih.gov/articles/PMC4632875/#ack1
Furukawa, M. F., & Menachemi, N. (2020). Electronic health records and patient outcomes: A review of the literature. Health Services Research, 55(S2), 238–254. https://doi.org/10.1111/1475-6773.13563
Heponiemi, T., Kujala, S., Vainiomäki, S., Kaihlanen, A. M., Gluschkoff, K., Vehko, T., & Hyppönen, H. (2021). Usability problems of electronic health records and their association with stress and well-being among Finnish physicians: Cross-sectional survey. JMIR Medical Informatics, 9(12), e29074. https://doi.org/10.2196/29074
Holden, R. J., & Karsh, B. T. (2016). The technology acceptance model: Its past and its future in health care. Journal of Biomedical Informatics, 43(1), 159–172. https://doi.org/10.1016/j.jbi.2009.07.002
Khairat, S., Burke, G., Archambault, H., Schwartz, T., Larson, J., & Ratwani, R. (2019). Perceived burden of EHRs on physicians at different stages of their careers. Applied Clinical Informatics, 10(2), 349–359. https://doi.org/10.1055/s-0039-1688754
Kruse, C. S., Stein, A., Thomas, H., & Kaur, H. (2018). The use of electronic health records to support population health: A systematic review of the literature. Journal of Medical Systems, 42(11), 214. https://doi.org/10.1007/s10916-018-1075-6
Kruse, C. S., Stein, A., Thomas, H., & Kaur, H. (2023). The impact of electronic health records on workflow and patient outcomes: A systematic review. Journal of Medical Systems, 47(2), 12. https://doi.org/10.1007/s10916-023-01846-7
Kutney-Lee, A., Sloane, D. M., & Aiken, L. H. (2021). Electronic health records and nurse-reported quality of care: A national study of nurses in the United States. Journal of Nursing Scholarship, 53(2), 133–141. https://doi.org/10.1111/jnu.12640
Laumer, S., Maier, C., Weitzel, T., & Eckhardt, A. (2021). The impact of electronic health records on efficiency, quality, and user satisfaction: A systematic review. Journal of the American Medical Informatics Association, 28(4), 808–818. https://doi.org/10.1093/jamia/ocaa273
Lee, S. (2022). Effects of electronic medical record quality on nurses’ perceived usefulness, ease of use, and system satisfaction. Healthcare Informatics Research, 28(3), 207–216. https://doi.org/10.4258/hir.2022.28.3.207
Lee, S., Park, J., & Kim, J. (2022). Factors influencing nurses’ acceptance of electronic health records: Extending the technology acceptance model. Healthcare Informatics Research, 28(3), 210–219. https://doi.org/10.4258/hir.2022.28.3.210
Medina-Martínez, J., González-García, A., & Morales-Asencio, J. M. (2023). Digital competence in nursing: A cross-sectional study of clinical practice adoption. Journal of Nursing Management, 31(2), 345–354. https://doi.org/10.1111/jonm.13788
Osei-Bonsu, P. E., Boateng, D., & Mensah, J. (2023). Continuous professional training and electronic health record utilization among nurses: Evidence from a multicenter study. BMC Nursing, 22(1), 147. https://doi.org/10.1186/s12912-023-01234-1
Rahimi, B., Vimarlund, V., & Timpka, T. (2018). Health information system implementation: A qualitative meta-analysis. Journal of Medical Systems, 42(3), 1–12. https://doi.org/10.1007/s10916-018-0901-0
Ramoo, V., Lai, N. M., Wong, L. P., Danaee, M., & Wong, P. F. (2023). Nurses’ perceptions, satisfaction, and barriers toward electronic medical records use: A cross-sectional survey. BMC Nursing, 22(1), 135. https://doi.org/10.1186/s12912-023-01208-7
Shan, R., Ding, J., & Li, S. (2023). Electronic health record usability and its association with nurse workload: A systematic review. International Journal of Nursing Studies, 144, 104482. https://doi.org/10.1016/j.ijnurstu.2023.104482
Shan, R., Ding, J., Yan, C., Zhang, Y., & Xu, Y. (2023). Barriers and facilitators to electronic health record adoption: A meta-synthesis of qualitative studies. BMC Health Services Research, 23, 765. https://doi.org/10.1186/s12913-023-09870-4
Top, M., Gider, Ö., & Taş, Y. (2021). Nurses’ perceptions of the impact of electronic health records on time efficiency and workflow. Journal of Nursing Management, 29(3), 405–414. https://doi.org/10.1111/jonm.13154
Venkatesh, V., Thong, J. Y., & Xu, X. (2016). Unified theory of acceptance and use of technology: A synthesis and the road ahead. Journal of the Association for Information Systems, 17(5), 328–376. https://doi.org/10.17705/1jais.00428
Wang, Y., Kung, L., & Byrd, T. A. (2021). Big data analytics: Understanding its capabilities and potential benefits for healthcare organizations. Technological Forecasting and Social Change, 126, 3–13. https://doi.org/10.1016/j.techfore.2020.120329
World Health Organization. (2020). State of the world’s nursing 2020: Investing in education, jobs and leadership. WHO Press. https://www.who.int/publications/i/item/9789240003279
Additional Files
Published
Issue
Section
License
Copyright (c) 2025 Maria Joana dela Cruz, Cheena Berber Mallari (Author)

This work is licensed under a Creative Commons Attribution 4.0 International License.
Articles in the APCORE Online Journal (AOJ) are published under the Creative Commons Attribution 4.0 International License (CC BY 4.0). Authors retain copyright and grant the journal the right of first publication, allowing others to share and adapt the work with proper attribution to the original author and source.
https://creativecommons.org/licenses/by/4.0/